
An infected blood scandal in Britain was no accident but the fault of doctors and a succession of governments that led to 3,000 deaths and thousands more contracting hepatitis or HIV, a public inquiry has found.
Inquiry chair Brian Langstaff said more than 30,000 people received infected blood and blood products in the 1970s and 1980s from Britain's state-funded National Health Service (NHS), destroying lives, dreams and families.
The government hid the truth to "save face and to save expense", he said, adding that the cover-up was "more subtle, more pervasive and more chilling in its implications" than any orchestrated conspiracy plot.
Prime Minister Rishi Sunak is expected to apologise on behalf of the state when he addresses the House of Commons later on Monday. Langstaff, a former High Court judge, received a standing ovation by campaigners as he delivered his findings.
The families of victims and survivors had sought justice for years and Langstaff, who led a near 6-year inquiry, said the scale of what happened was both horrifying and astonishing.
In some cases, blood products made from donations from US prisoners or other high-risk groups were used on children, infecting them with HIV or hepatitis C, long after the risks were known.
Other victims were used in medical trials without their knowledge or consent. Those who contracted HIV were often shunned by their communities afterwards.
"This disaster was not an accident," Langstaff said. "The infections happened because those in authority - doctors, the blood services and successive governments - did not put patient safety first."
He said proper compensation must now be paid.
The use of infected blood has resulted in thousands of victims in the United States, France, Canada and other countries.
The British government, which in 2015 said it was "something that never should have happened", agreed in 2022 to make an interim payment of 100,000 pounds ($126,990) to those affected.
Clive Smith, chair of the Haemophilia Society, said the scandal had rocked trust in the medical establishment. "(It) really challenges the trust that we put in people to look after us, to do their best and to protect us," he told reporters.
The infected blood and blood products, some of which were imported from the United States, were used for transfusions, which were not always clinically needed, and as treatments for bleeding disorders like haemophilia.
Haemophiliacs received Factor 8 concentrates which carried a paticularly high risk of infection.
Some of the concentrates were infected with HIV in the 1980s, the inquiry said, but authorities failed to switch to safer alternatives, and they decided in July 1983, a year after risks were apparent, not to suspend their importation.
Systemic failures resulted in between 80 and 100 people becoming infected with HIV by transfusion, the inquiry found, and about 26,800 were infected with Hepatitis C, often from receiving blood after childbirth or an operation.
Both groups were failed by doctors' complacency about Hepatitis C and their slowness to respond to the risks of AIDS, it said, compounded by an absence of meaningful apology or redress.
"It will be astonishing to anyone who reads this report that these events could have happened in the UK," Langstaff said.
The British inquiry, which started in 2018, does not have the power to recommend prosecutions.
In France, former health minister Edmond Herve was convicted in 1999 for his role in the scandal, but he received no punishment. Michel Garretta, the director of France's national blood centre, received a four-year sentence.



 At least 15 dead in Guatemala bus accident
At least 15 dead in Guatemala bus accident
 Pakistan's former central bank head Shamshad Akhtar dies at 71
Pakistan's former central bank head Shamshad Akhtar dies at 71
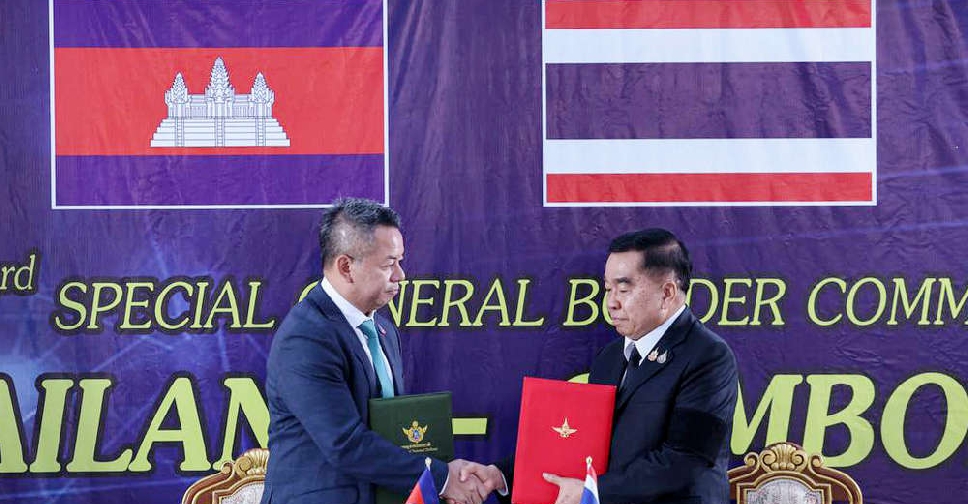 Thailand and Cambodia sign truce to halt fierce border conflict
Thailand and Cambodia sign truce to halt fierce border conflict
 Winter storm bears down on US Northeast, disrupting airline travel
Winter storm bears down on US Northeast, disrupting airline travel
 Russian drones, missiles pound Ukraine ahead of Zelenskyy-Trump meeting
Russian drones, missiles pound Ukraine ahead of Zelenskyy-Trump meeting






